This last post in a series from our friend Professor Sonia Grover steps back a little to think about what makes periods happen, and in the process, discusses another cause for pelvic pain. This time, a pain that happens halfway between periods – ovulation pain, or mid-cycle pain. Our thanks to Professor Grover for such an informative series!
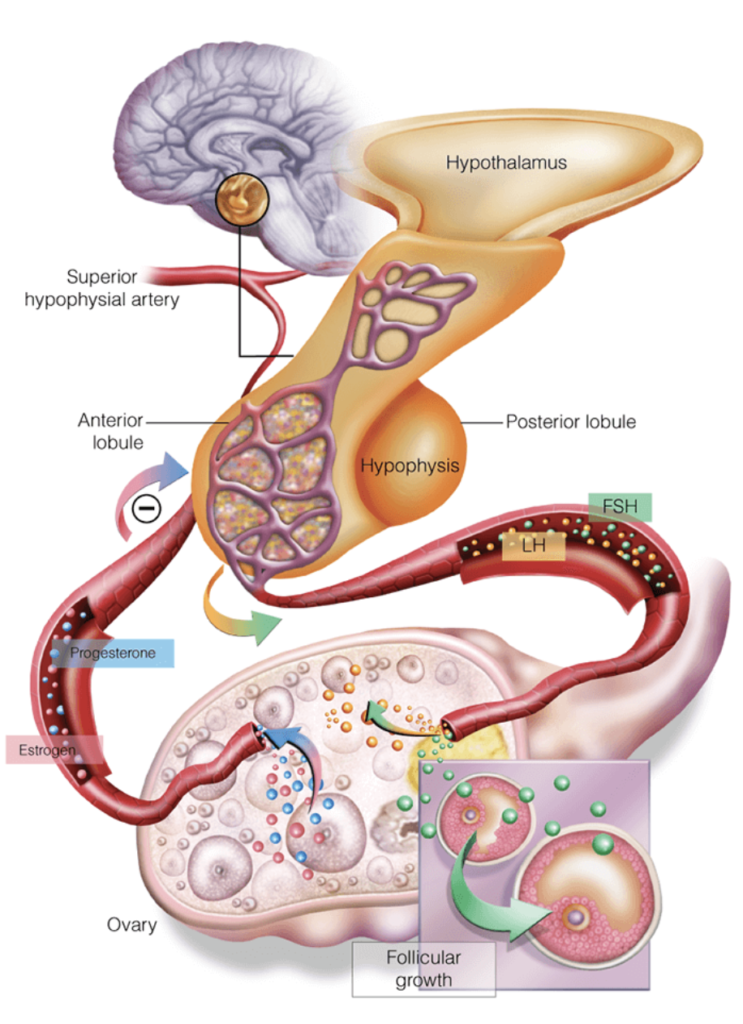
The hypothalamic-pituitary-ovarian (HPO) axis
The messages (hormones) to make periods happen originate in the brain – with messages coming from one part (the hypothalamus) going to another part of the brain (the pituitary) – which then sends messages to the ovaries. The ovaries, which contain the eggs and the supporting set of surrounding cells, then produce the key hormones we associate with being women: oestrogens and progesterones.
An irregular start
Normally the messages from the brain start in a disorganised manner – so that things simply ‘switch on’. Usually, a bit later, a clock centre (in the brain) begins to coordinate things, so that periods are regular and an egg is released. When this happens, the second hormone (progesterone) is then produced. This explains why periods are usually irregular to start with – and can remain irregular for one to three or even four years. Strangely, in girls whose periods start younger (eg at 10 years of age), the periods become regular sooner; whereas those who start their periods later (eg., 15 or 16 years), it can take the four years before the periods become regular.
With organised hormones, the release of an egg involves the development of an ovulation follicle or cyst. I need to sidetrack here, as a cyst in medical language is any roundish-shaped structure filled with fluid. An eyeball is actually a cyst!! And the vast majority of ‘cysts’ on the ovaries are actually ‘Congratulations, your ovaries are working, I hope you are using contraception if there is a boy around-cyst’.
This ovulation cyst/follicle is usually about 3-4cm in size and has a fantastic blood supply around its outer surface. It is through this highly vascular surface that the egg is ‘released’, meaning it leaves this hormone-filled cyst space, and ‘wiggles’ through the cyst surface and then heads off to the fallopian tube drawn by chemotaxic forces (a bit like a magnet), where it is hoping to meet sperm. Around the time of the release of the egg, it is well recognised that pain may occur. It is unclear what exactly causes this pain- whether it relates to the stretching of the ovary and cyst surface, or if it is the leakage/spillage of some of the hormone fluid (which could be 7-10 mls, that is two tablespoons of hormone fluid), or whether it is the chemicals (yes, these include those wonderful inflammatory cytokines), that assist in the egg making a path through the follicle/cyst wall is unclear.
When the egg passes through this highly vascular follicle surface, some disruption to the blood vessels may also occur and this may cause some bleeding. This bleeding can then either further expand the follicle/cyst, so that it becomes a 5-6 cm blood filled cyst, or haemorrhagic corpus luteum (in medical language), on the ovary. This haemorrhagic corpus luteum can look very similar to an endometrioma on ultrasound. Or the bleeding dribbles into the pelvis and irritates the outer bladder surface, bowel surface and pelvic floor. Whichever way, this process can be painful. The first is effectively like a big bruise on the ovary, and like a bruise elsewhere, it is painful and will last a few weeks before it resolves. The body really is clever in the way it can reabsorb bruising and bleeding, isn’t it? This bleeding associated with ovulation is likely to be worse in women who already suffer from heavy periods as they are the ones who have bodies that ‘like’ to bleed!
The end result of all of this can be ovulation pain or mid-cycle pain
This is not a great addition to the pelvic pain issues that someone may already be experiencing with their period pain. But again, this too can be easily fixed. Although the hormonal intrauterine system (Mirena) works well for painful and heavy periods, it does not do so well with ovulation pain – as the hormonal effect is localised to the uterus. Fortunately, the pill or other hormonal approaches to stop periods, will also stop ovulation (as will pregnancy and breastfeeding) and thus prevent this pain.
– Sonia Grover

Professor Sonia Grover has extensive experience in paediatric and adolescent gynaecology having worked in this field for over 20 years. She has been instrumental in establishing this subspecialty in Australia as well as in Asia and internationally. Professor Grover’s clinical interests include all aspects of young women’s reproductive health – including menstrual problems (excessive bleeding and/or pain), amenorrhoea, ovarian problems, congenital anomalies affecting the reproductive tract and reproductive hormones and the cyclic exacerbation of ‘non-gynaecological symptoms’ including cyclic seizures, asthma, and chronic fatigue. Professor Grover’s ResearchGate profile here.
Sonia’s five-blog series:
#1: Period Pain
#2: Periods are extraordinary events, and it’s ok to skip them
#3: Heavy periods and retrograde bleeding
#4: Understanding the common by learning from the rare
#5: Ovulation Pain
Feature image adapted from Freepik.

your post is very interesting to read.it’s very informative and helpful.This article was extremely well done and sooo accurate Usually, I never comment on blogs but your article is so convincing that I never stop myself to say something about it. You’re doing a great job, Keep it up.