Continuing on our sequence of stories from neuroanatomy …
Clinicians know that persistent pain experienced around the ischial tuberosity and subgluteal space can sometimes be tricky to sort out. There is a fear factor here too – the athlete pondering if their hammie is going to go and those who google “piriformis syndrome” will find many treatments offered for something not fully understood.
Over the years, I have thrown every manual test known to manual therapy at the bum (or butt for our American friends) in an attempt to find local culprits, though in recent years, the introduction of central sensitisation into reasoning has lessened the need for relentless testing.
A recent paper by Bäumer et al. (2015) excited my clinical pattern memory book. I have noted that in the presence of bum area pain, while a straight leg raise may not show much, if you do it with ankle plantar flexion inversion (ie load fibular divisions), the problem appears to be elicited. However, in the same person, if you do the SLR with ankle dorsiflexion/eversion (ie loading tibial divisions), it all seems fine. And vice versa too – a tibial division loaded SLR can reproduce bum area pain, but not the fibular loaded SLR.
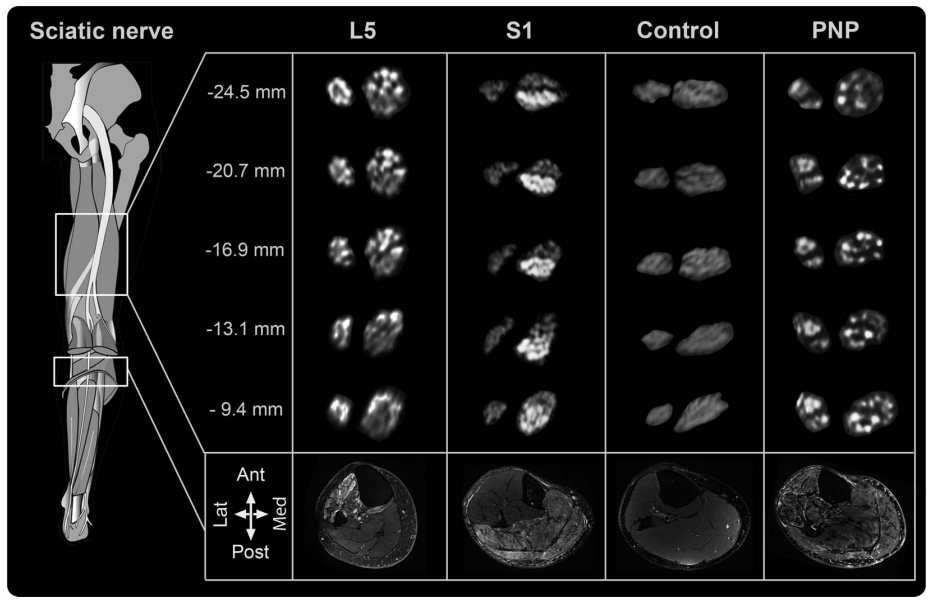
The Bäumer et al. (2015) paper provides in-vivo evidence of a distinct somatopic pattern within the sciatic nerve. In other words, the nerve bundles from the L5 and S1 roots were separate in the nerve. While there is a bit of nerve fibre intermingling, the nerve topography is more cable like than a mixed plexiform structure. L5 bundles are more anterolateral within the nerve and S1 posteromedial (see image below). So the nerve is more like a sheath around separate bundles (fascicles). It’s not all twisted up inside the nerve as many of us may have thought.
So what can we take from these observations and the experimental findings:
- In the case of buttock pain, especially where there are hints of neurogenic involvement, it is worth performing tests via both divisions of the sciatic nerve – try DF/eversion and PF/inversion while in SLR
- Pathology leading to mid axon discharge could come from one division and not the other
- The divisions/bundles can move in relation to each other. Maybe a bleed or inflammation within the sciatic sheath can hinder this movement.
- maybe you can perform a sciatic interfascicular mobilisation (sounds sexy, eh?). That is what I thought I was doing in one of my patients. In hip flexion, work knee extension in plantar flexion/inversion and then work it in dorsiflexion/eversion (as in the image above).
Happy mobilising, share your thoughts.
– David
Useful Links
Bodily Relearning, Boyd BS
Neurodynamic techniques Handbook & Videos, Butler DS
The Sensitive Nervous System, Butler DS

Great article, Dave!
Sounds reasonable. Can remember a few cases where incuding neck flexion to inversion-eversion alternatives seamed to improve the treatment trials.
Thanks a lot for undefatigable and generous information!
Thanks Russell and Dan,
That is interesting Dan. When the leg is in SLR, especially with the foot in plantarflexion and inversion, neck flexion will alter responses in about half those tested.
Cheers
David
I remember a lady had a buttock pain which was reproduced in SLR hip slightly externally rotated, but with 100 knee flexion, and ankle in DF/Inv. The pain was a bit relieved with PF/Ev. I am not sure if this is related to the neuroanatomical deviation of the sciatic nerve pathway through the piriformis (neural container issues).
I am also astonished by the study finding. This “intrafascicular” pattern facilitate better understanding of buttock pain. It could be worthy to check the effect of lumber spine flexion and extension during testing.
Thank you for sharing your thoughts.
Hi Ahmad,
It is intriguing – foot position will often alter responses such as you have described. They will often alter responses even in a Prone Knee Bend. Some of this may be due to loading on sensitive neural structures, other times it may relate to distraction away from the body part where pain is experienced.
Best wishes
David